Overview
Teaching in the clinical setting is perhaps simultaneously the greatest joy and greatest challenge of medicine. Often, we feel rushed and it is difficult to incorporate impactful clinical teaching into your busy clinic or hospital day.
Effective clinical teaching takes practice and cannot simply be summarized in this module. However, we present some key considerations for clinical educators and their teaching skill development.

“Medicine is learned by the bedside and not in the classroom.” - Sir William Osler
Key Learning Points
- Setting expectations with your learners is necessary for a high-quality experience.
- Clinical teaching doesn’t require a lot of time; you can use as little as one minute for an impactful teaching moment.
- Applying the principles of observation and effective feedback is important and provides learners with instruction on clinical skills.

Guiding Principles
In this module, we will review the importance of setting expectations for learners in your clinical environment, considerations of what, where and how to teach, and how to embed assessment and feedback into your clinical practice.
Set the Ground Rules
It is important to prioritize a discussion with your team early in your time together to make all members aware of expectations - expectations you have of them and expectations they can have of you.
- Understand the goals and objectives of the rotation: For all learners under your supervision, familiarize yourself with goals and objectives. These goals and objectives will be both formal and informal, those dictated by the medical school, residency or fellowship program, and those goals learners set for themselves for a particular clinical experience.
- Communicate your expectations: These expectations can be team-wide, but you will also have learner-specific expectations. Communicate your expectations not just for patient care, but for other aspects of their experience, including time management, professionalism, and interprofessional communication. Be sure to share your rationale for your expectations so learners can understand their importance and applicability to future practice.
- Plan your teaching time: Discuss with learners how you plan to teach them. Decide whether and when you will have dedicated teaching sessions, if plan to teach at the bedside, through direct observation, etc.
- Be transparent about evaluation: Familiarize yourself with formal medical school, residency, or fellowship evaluations to guide your direct observation and feedback. If you have additional evaluative measures, be sure to communicate them with learners at the beginning of the rotation.
Clinical Teaching - The What and Where
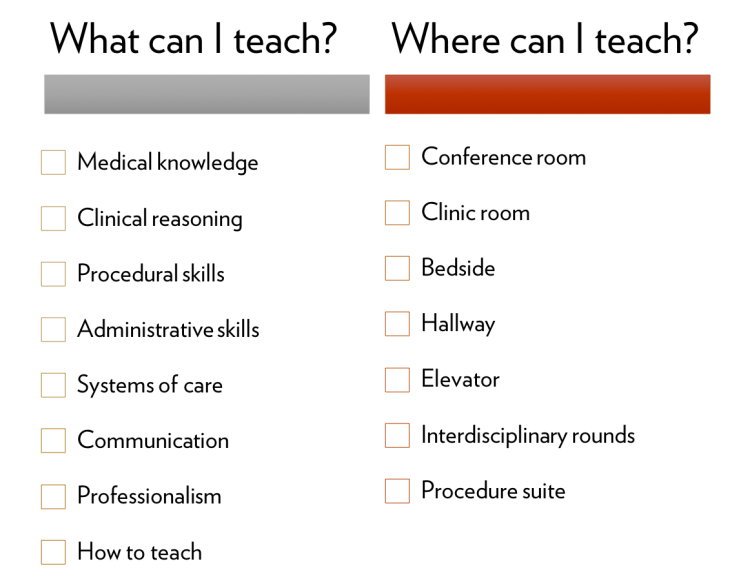
Teaching in the clinical setting is not limited to teaching medical knowledge in a conference room. Consider providing instruction on a variety of topics and skills necessary for patient care and leverage time with your team in non-traditional settings, such as hallways and elevators.
Clinical Teaching - The How
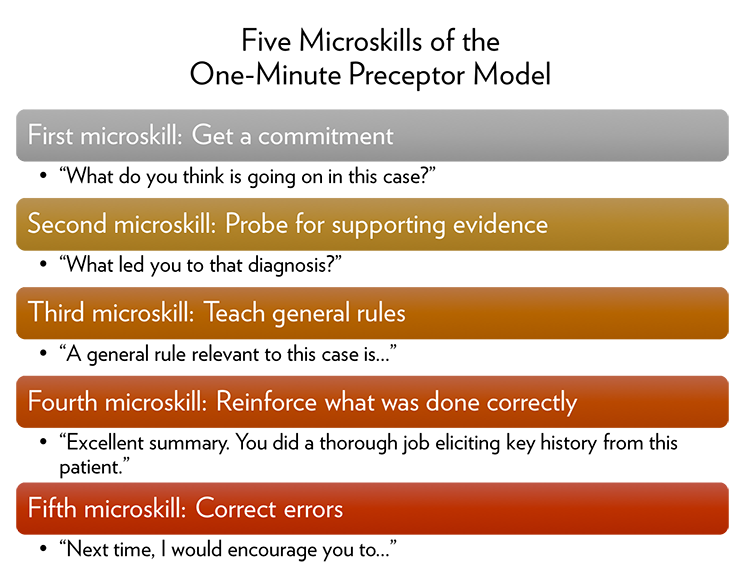
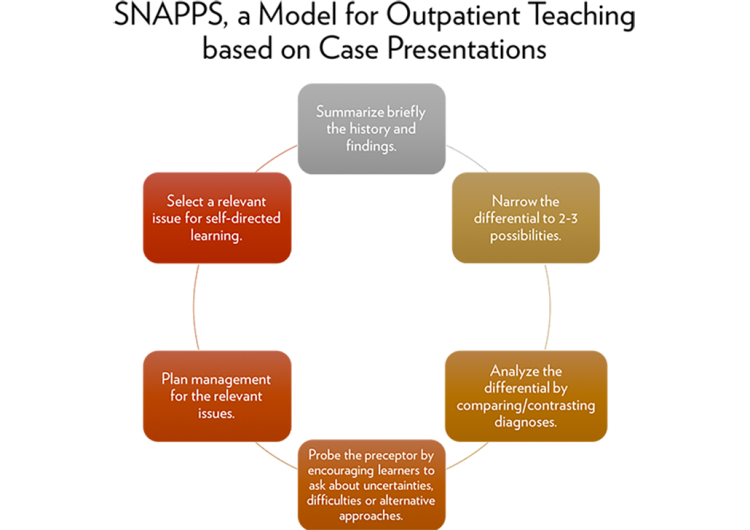
Clinical teaching is an art perfected over years. There are two well-established tools educators can rely on to guide them in brief teaching encounters in the clinical setting: the One-Minute Preceptor and SNAPPS. The SNAPPS model is more often applied in the outpatient setting, though both are useful constructs for all clinical educators.
Embedding Assessment and Feedback into Clinical Teaching
Direct observation provides robust opportunities for meaningful feedback on patient care skills for learners of all levels.
Given our clinical teams are mixed-learner level, it can be challenging to assess the competence of an individual learner to tailor teaching to an appropriate level. Consider the following questions to ask of learners to gauge their clinical acumen:
- How many ward rotations have you had?
- How much time have you spent in your continuity clinic?
- What are you currently working on?
- How can I help you get to your next step?
It can be useful to consider learners in the RIME construct, which can help you provide attainable next steps to learners at different levels.
- Reporter: Learner provides clear and organized presentations.
- Interpreter: Learner develops a differential diagnosis and next steps.
- Manager: Learner can apply literature to a given patient.
- Educator: Learner is self-directed and teaches others.
Consider using the COACH program developed by our colleagues in the Department of Medicine to guide direct observation and feedback.
Wrap Up
To be an effective clinical educator, communicate your expectations, employ direct observation and feedback, and leverage brief amounts of time for teaching points.
Other Resources
Alguire, P.C., DeWitt, D.E., Pinsky, L.E., and Ferenchick, G.S. Teaching in Your Office: ACP Teaching Medicine Series. American College of Physicians, 2008.
Orlander, J.D. "Twelve tips for use of white board in clinical teaching: Reviving the chalk talk," Medical Teacher. 2007. 29: 89-92.
References
Neher, J. O., Gordon, K. C., Meyer, B., and Stevens, N. "A five-step 'microskills' model of clinical teaching," The Journal of the American Board of Family Practice. 1992. 5(4), 419–424.
Pangaro, L. "A new vocabulary and other innovations for improving descriptive in-training evaluations," Academic Medicine. 1999. 74: 1203-7.
Pascoe, J. M., Nixon, J., and Lang, V. J. "Maximizing teaching on the wards: review and application of the One-Minute Preceptor and SNAPPS models," Journal of Hospital Medicine. 2015. 10(2), 125–130.
Reilly, J. B., Bennett, N., Fosnocht, K., Williams, K., Kangovi, S., Jackson, R., and Ende, J. "Redesigning rounds: towards a more purposeful approach to inpatient teaching and learning," Academic Medicine. 2015. 90(4), 450-453.
Seki, M., Otaki, J., Breugelmans, R., Komoda, T., Nagata-Kobayashi, S., Akaishi, Y., and Izumi, M. "How do case presentation teaching methods affect learning outcomes?-SNAPPS and the One-Minute preceptor," BMC Medical Education. 2016. 16.
Wolpaw, T. M., Wolpaw, D. R., and Papp, K. K. "SNAPPS: a learner-centered model for outpatient education," Academic Medicine: Journal of the Association of American Medical Colleges. 2003. 78(9), 893–898.
Wiese, J. Teaching in the Hospital: ACP Teaching Medicine Series. American College of Physicians, 2010.