Research by Dr. Amy Kind helps target federal diabetes intervention program
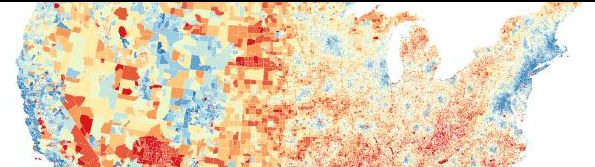
Research by Dr. Amy Kind that identified a measure of socioeconomic disadvantage is being used by a federal program to better target community public health programs aimed at improving the health and quality of life of people living with diabetes and pre-diabetes. Above, map provided by Dr. Kind and Dr. William Buckingham of the Applied Population Laboratory with color-coded representation of Area Deprivation Index (ADI). The colors represent ADI deciles, with blue indicating least disadvantaged and red indicating most disadvantaged areas. Urban block groups are less visually apparent due to their small geographic size.
Where you live has a major impact on your health.
As that simple idea gains more traction in public health research, the Centers for Medicare and Medicaid Services (CMS) is now employing a novel tool to target disparities in diabetes care.
Amy Kind, MD, PhD, associate professor, Geriatrics and Gerontology, and her team have refined the Area Deprivation Index (ADI), which allows neighborhoods to be ranked by socioeconomic disadvantage based on 17 US census indicators such as level of education, housing costs, unemployment rates, income levels, and housing quality markers—including factors like crowding. In 2014, she published findings showing seniors from at-risk neighborhoods are more likely to experience hospital readmission after being treated for illnesses such as congestive heart failure than those from less disadvantaged neighborhoods. In that work, Dr. Kind’s team matched ADI data in more than 30 million US nine-digit zip code regions with Medicare claims and other healthcare data. Their analysis allowed a very granular view of socioeconomic disadvantage—down to a census block group, which is an area ranging from 600 to 3000 people—and linked it to information about medical outcomes. Recently, as part of a study funded by the National Institutes of Health on Minority Heath and Health Disparities, Dr. Kind’s team updated these metrics for every neighborhood in the US.
CMS program leaders took note of the work and will now use these data to target diabetes education efforts to seniors residing in the most disadvantaged areas (in addition to targeting traditional individual disparities). The Everyone with Diabetes Counts (EDC) program, which provides diabetes self-management education to medically underserved seniors, will use the ADI tool from Dr. Kind’s team to add neighborhoods and communities in each state that had not previously been identified for inclusion, allowing EDC’s diabetes prevention and outreach classes to reach additional seniors in need. [Read more]
“We are thrilled that our research has contributed in a meaningful way to this critical policy initiative. In the coming year we will be making these updated metrics freely available to the public for all to use in health, research, policy and other community initiatives,” said Dr. Kind.
According to the Centers for Disease Control and Prevention, 29.1 million Americans have diabetes and another 86 million have prediabetes (a precursor of diabetes). The Centers for Disease Control’s 2014 national diabetes statistical report also states one in 10 health care dollars is spent treating diabetes and its complications. Additionally, 30 percent of those with a known diagnosis of diabetes require more than two overnight hospitalizations per year.
Resources:
-
Everyone with Diabetes Counts
- Kind AJH, et al. 2014. Neighborhood Socioeconomic Disadvantage and 30-Day Rehospitalization: A Retrospective Cohort Study. Ann Intern Med. 161(11):765-774.