Early Detection and Prevention of Alzheimer’s Disease and Related Disorders
Sterling Johnson, PhD, is a clinical neuropsychologist whose research focuses on brain function in Alzheimer’s disease and related disorders.
Dr. Johnson leads WRAP: Wisconsin Registry for Alzheimer's Prevention, a longitudinal cohort study of 1700+ people at varying levels of risk for sporadic Alzheimer's disease.

Active Projects
- Pre-Symptomatic Detection of Alzheimer’s Disease: A Window for Prevention
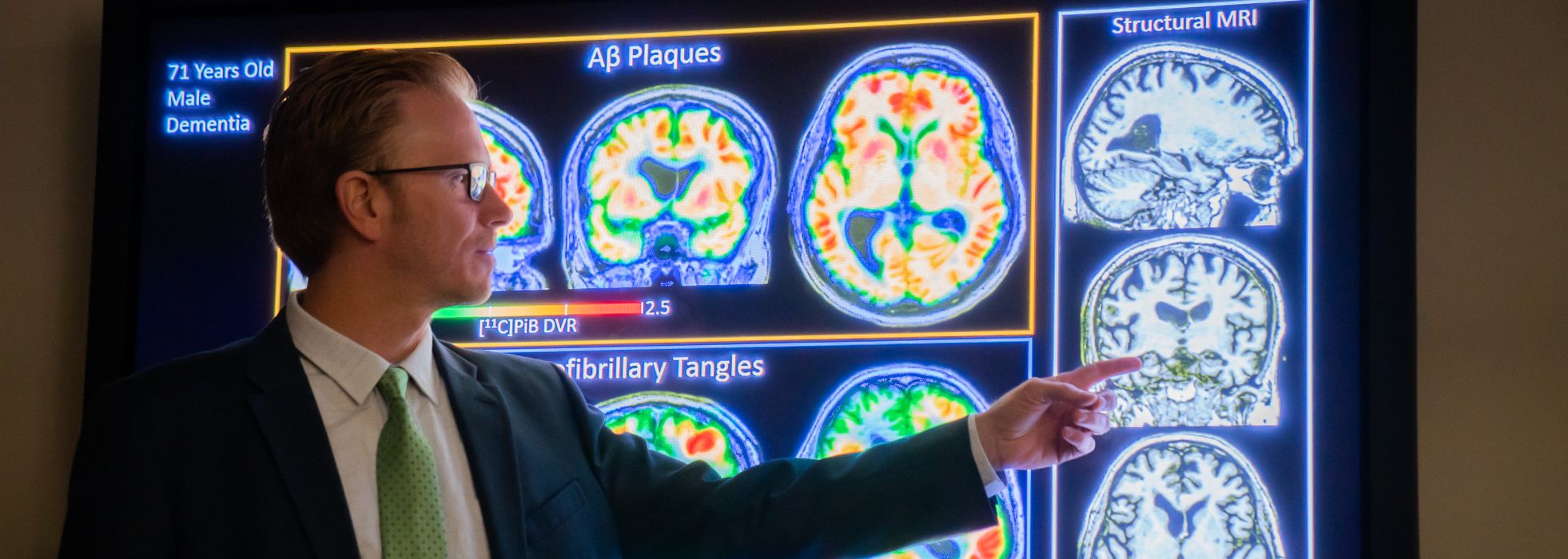
Detecting AD prior to its symptoms of cognitive decline is a prerequisite for effective prevention. In the WRAP study, which follows healthy middle-aged volunteers who are at increased risk for AD, we are focused on identifying when AD begins at the level of the individual person. We do this with specialized PET imaging biomarkers of amyloid plaques and neurofibrillary tangles as well as cerebrospinal fluid (CSF) and blood-based biomarkers.
We are also focused on identifying the earliest manifestation of cognitive decline, which may actually be detectable several years before a clinical diagnosis of mild cognitive impairment or dementia. Our work has shown that the presymptomatic stage of AD lasts at least as long as the cognitively impaired stage, providing a lengthy window of opportunity for secondary prevention research.
- Risk Factors for Alzheimer’s Disease
Why do some people develop symptoms of AD earlier than others? What role do health and lifestyle factors play in the development of AD?
The WRAP study collects a plethora of health and lifestyle factors on our participants and Johnson’s lab and several other collaborating research teams are focused on identifying modifiable factors that increase or decrease risk for Alzheimer’s disease proteinopathy and eventual cognitive decline.
- Multi-Etiology Cognitive Impairment
Does Alzheimer’s disease occur by itself? Our success in identifying the onset age of AD proteinopathy at the person-level has created the opportunity to learn what else may be going on in the brain that may be contributing to cognitive decline. The neuropathologists tell us that what we presume to be Alzheimer’s disease is actually often (over 60% of the time) a mix of etiologies. AD may co-occur with vascular disease, alpha synuclein proteinopathy, and/or TDP43 proteinopathy.
Our field lacks the tools to identify multi-etiology cognitive impairment (MECI) and antecedent states in-vivo that present clinically as presumed AD. This has hindered progress in identifying antemortem constituent pathologies in individuals, and their stage of progression. Such knowledge would greatly inform clinical trial participant selection, improve diagnosis and prognosis, and accelerate biomarker and treatment discovery.